A new milestone
Today, we’re proud to share that our new paper, “Depression and Anxiety Outcomes in a Technology-Enabled Psychotherapy Practice: Retrospective Cohort Study,” has been published in JMIR Formative Research. This marks Two Chairs’ second peer-reviewed publication, further strengthening a growing body of evidence on what high-quality, measurement-driven behavioral health care can achieve at scale. It builds directly on our December 2024 peer-reviewed study, which showed that rigorous training and implementation of Measurement-Based Care (MBC) improved clinical outcomes by 24% across our practice.
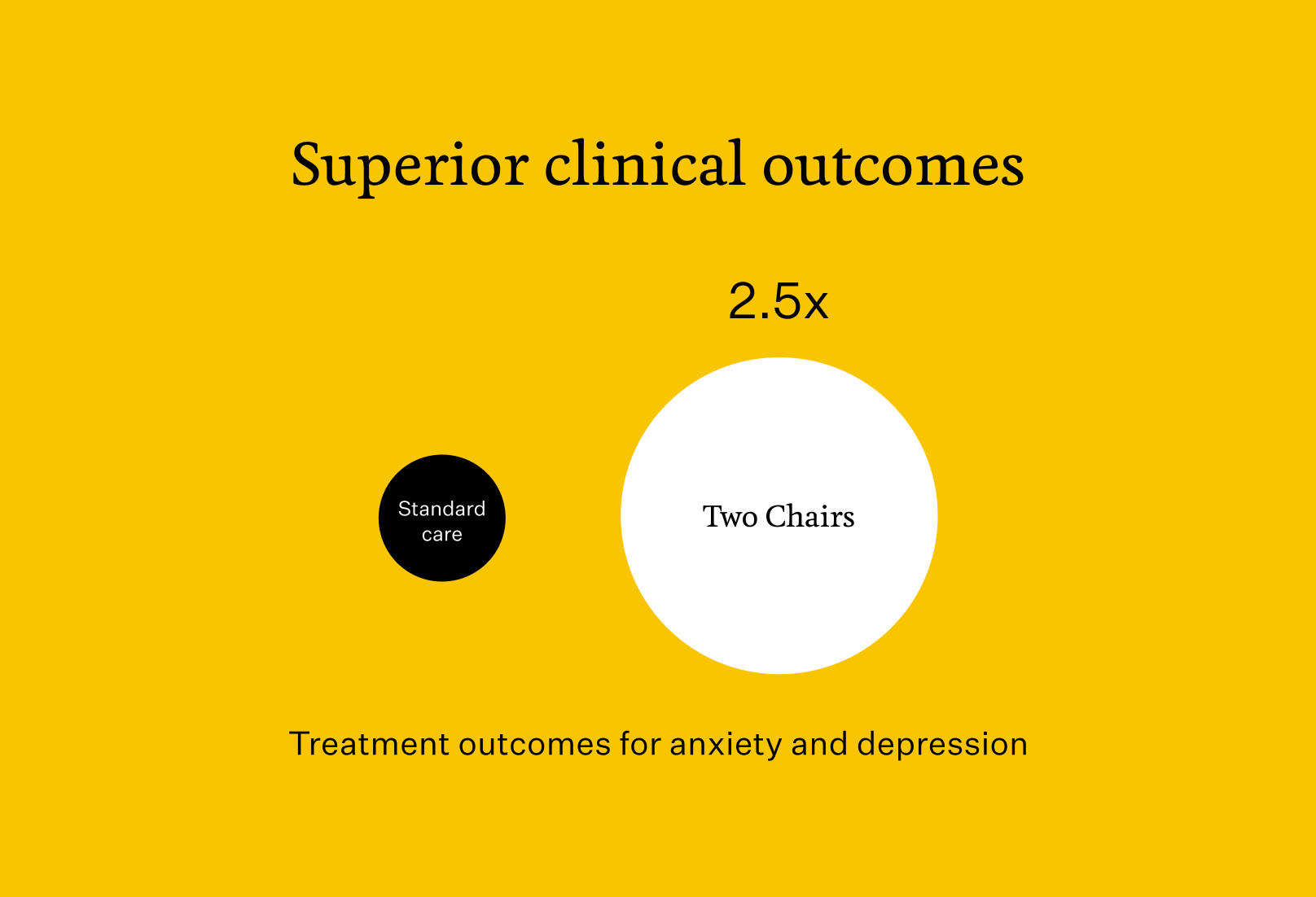
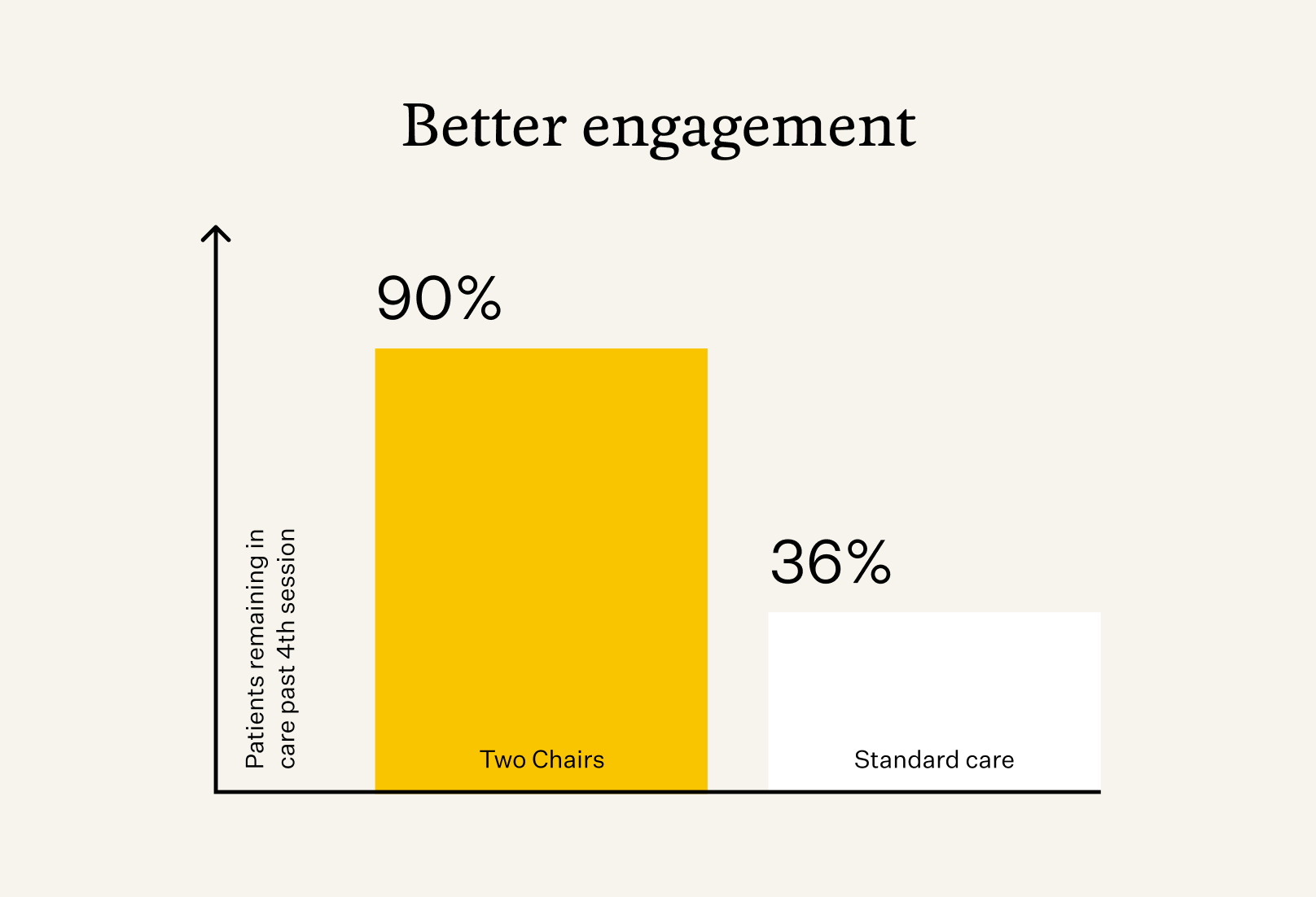
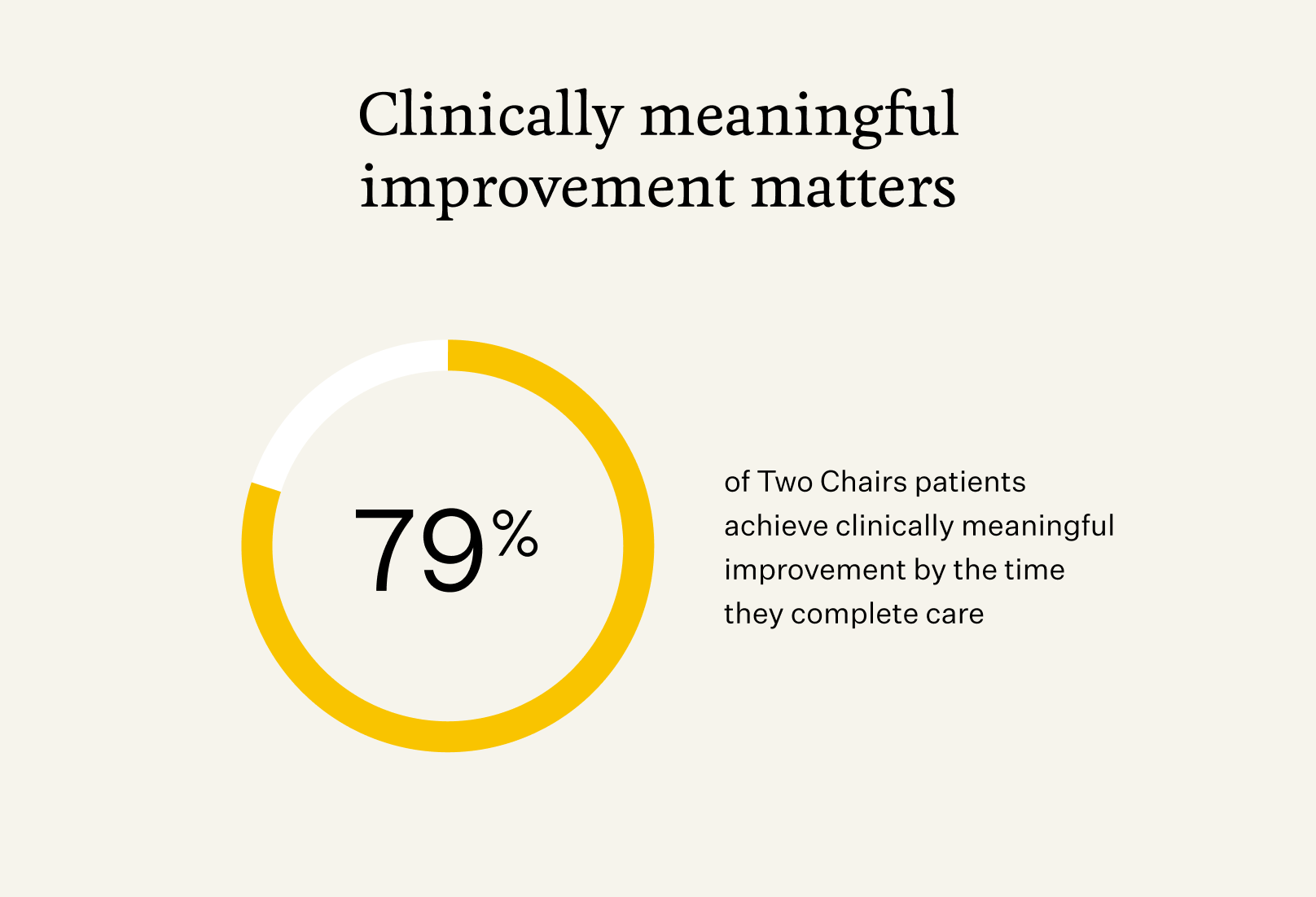
It’s one of the first large-scale analyses of how a technology-enabled model performs in everyday clinical practice, and the results are remarkable: patients at Two Chairs experienced outcomes up to 2.5x better than standard care for anxiety and depression. 90% stayed engaged through the fourth session and nearly 80% achieved clinically significant improvement by the time they completed care. Together with our prior MBC findings, this research shows not only that MBC works in theory, but that it can be implemented consistently and drive better outcomes at scale.
As the first author on this study and head of our research department, I find it deeply fulfilling to see these results — not just because they validate our model, but because they show the real impact of our care for people who are suffering. In academia or the lab, we rarely get to see the direct impact of our work, because the path from research to real-world impact is so long. At an organization like Two Chairs, the impact is immediate. We’re working with hundreds of clinicians and thousands of patients, and we can see directly that those patients are getting better. That makes me proud — not just as a researcher, but as part of a team making a real difference.
The core problem in behavioral health
Quality of care is one of the biggest problems in the mental health space. It starts at the beginning; the most common number of therapy sessions is one. That means many people, when they finally work up the courage to seek help, don’t get what they need and never return. They miss the chance to improve. Clinicians lose the opportunity to help. And health plans spend money without seeing meaningful outcomes for their members.
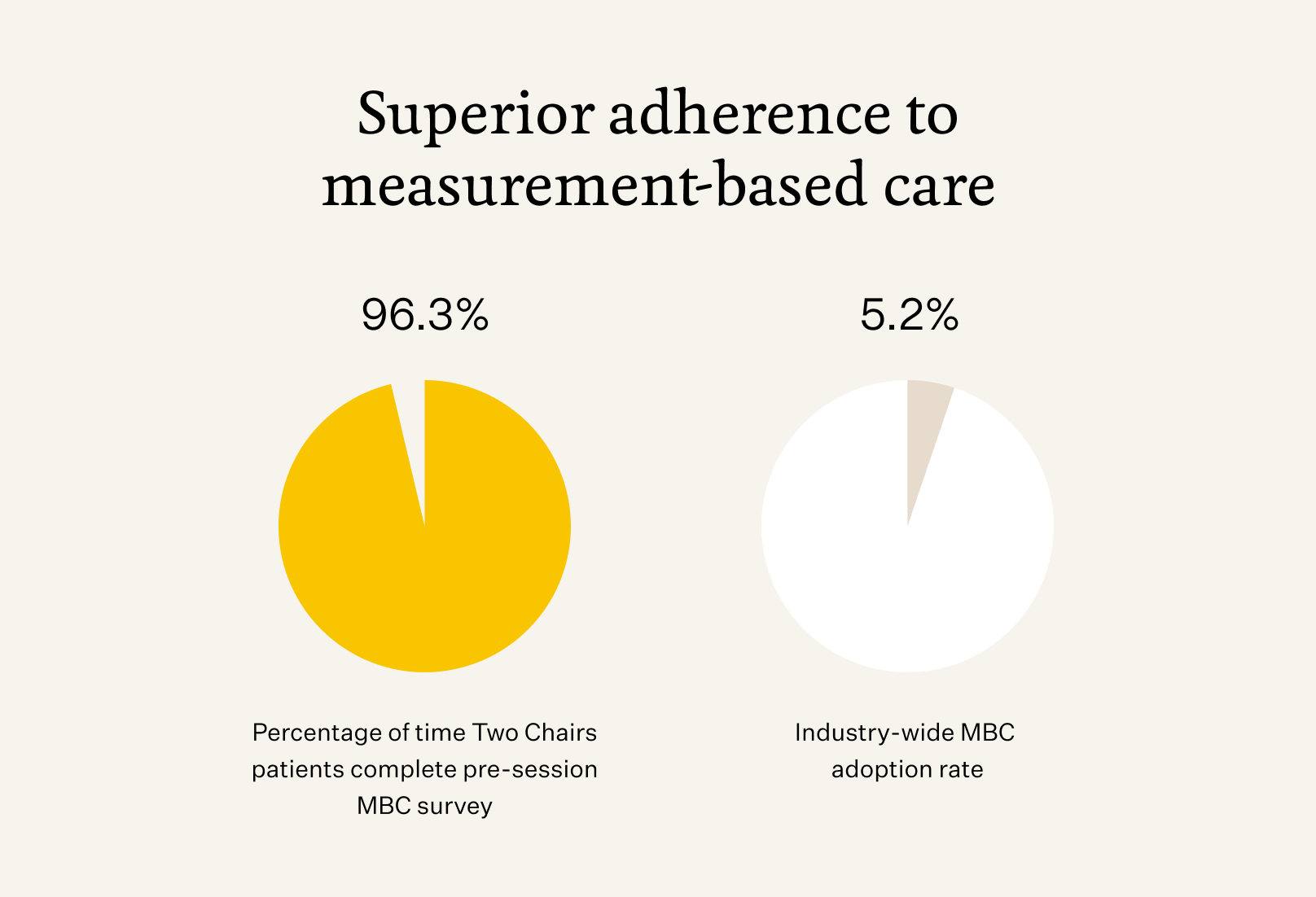
The other problem is that care may be of poor quality, and our key stakeholders – patients, health plans, even clinicians – would hardly know. As an industry, we don’t consistently measure our outcomes or use this information to guide clinical practice. Fewer than 20% of providers use measurement-based care (MBC) at all and even fewer use it regularly (~5%). Our earlier peer-reviewed research showed just how much this gap matters: when MBC is implemented consistently, outcomes improve materially.
Patients deserve more than a guess. They deserve to know if care is helping them. Clinicians deserve feedback to guide their work. And health plans deserve proof that care is making an impact.
The problem we’re solving
At Two Chairs, we’ve built a care model designed to close those gaps:
- Reduce dropout by focusing on strong therapist–client matching and early engagement
- Support clinicians with technology and clinical decision support so MBC is easy and consistent
- Provide health plans with transparent, reliable data on outcomes
Not getting it right the first time really matters. When people drop out early, they may never try again, and that’s a missed opportunity to get better. Our system is helping people stay in care and get an adequate dose of therapy 90% of the time, and that means more people are actually improving. Our prior MBC study demonstrated that when clinicians are trained and supported to use measurement consistently, outcomes improve across nearly every therapist. This new research shows what happens when that foundation is applied across a scaled, technology-enabled care model.
The study and its findings
The study reviewed nearly 3,000 patients who began care with us in the first half of 2024.
Here’s what we found:
- Outcomes are 2 to 2.5x better than published outcomes for standard care of anxiety and depression.
- 90% of patients stayed through their fourth session (vs. <36% in standard care).
- 96% of measurement surveys completed, showing that nearly all clinicians are adhering to MBC practices (vs. 5% industry-wide).
- 79% of patients achieved clinically significant improvement in anxiety and depression by the time they completed care.
The standout for me is adherence to MBC. Ninety-six percent of the surveys we send out are completed. That means 96% of the time, clinicians are getting feedback on client progress, the therapeutic relationship, and quality of life. This level of consistency mirrors what we saw in our earlier MBC-focused paper, where structured training and implementation led to improved outcomes across 95% of therapists.You just don’t see that in regular practice – and it shows the strengths of the model that we’re built at Two Chairs.
That level of adherence is what sets the stage for everything else — patients improving, clinicians growing, and payers knowing the care they’re supporting is effective.
Why it matters
For patients, this matters because you deserve to know that therapy can work — and to see your own progress in real time. Most practices don’t offer that.
For clinicians, this means greater confidence and professional growth. If they’re using the tools we provide and engaging with feedback, they can see they’re making a difference. That’s rewarding, and it makes the work more sustainable.
For payers, this is about accountability. Too often, health plans are blind to the quality of care they’re paying for. With MBC built into our model, we can show them the outcomes of our care. That’s rare in this field.
If you go to an oncologist, you know they’ll follow evidence-based standards for care. Mental health should be no different. Across two peer-reviewed studies, we’ve now shown that consistent measurement and clinician-supported technology can materially improve outcomes in real-world psychotherapy.
The takeaway
We know that access to therapy matters. But outcomes matter more.
This study shows what’s possible when you combine strong client–therapist matching, consistent measurement, and a supportive clinical model. Our earlier MBC research showed that measurement works. This new study shows what happens when it’s implemented reliably and supported by technology at scale.Patients stay in care, clinicians feel more effective, and health plans know the care they’re investing in is delivering results.
If you’re suffering and you go to therapy, you deserve to know you’re getting the highest-quality care possible. And you deserve proof that you’re getting better.
That’s the standard Two Chairs is working to set — for patients, providers, and payers.
Research as a foundation
This paper is part of a broader research commitment at Two Chairs. Everything we build — from our care model to clinician training to purpose-built technology — is grounded in evidence and evaluated through real-world outcomes. With two peer-reviewed studies now demonstrating the impact of consistent measurement and a technology-enabled clinical model, we’re contributing concrete evidence to a field that has long lacked accountability.
By publishing peer-reviewed research, we aim to advance the field, contribute transparent data on what works, and continue learning how to deliver high-quality psychotherapy at scale.
Nick Forand, PhD, is Head of Clinical Innovation and Research at Two Chairs and first author of “Depression and Anxiety Outcomes After Measurement-Based Care in a Technology-Enabled Psychotherapy Practice at Scale: Retrospective Cohort Study,” published in JMIR Formative Research.





