Measurement-based care has existed for decades, but only recently has it become behavioral health’s favorite buzzword. In the past year alone, nearly every company has claimed they “do MBC.” At the Behavioral Health Tech conference last month, it dominated the conversation. Payers want it, and providers say they deliver it.
But here’s the truth: most of what’s being marketed as MBC is not MBC. Not clinically. Not structurally. And not in a way that creates real behavioral change or measurable outcomes.
This week, Two Chairs published new peer-reviewed research in Frontiers in Health Services showing what happens when MBC is implemented as it was designed — not as a checkbox or product feature, but as a full clinical program rooted in training, accountability, and implementation science. Before getting to the results, it’s worth explaining why most MBC efforts fall short.
What I Heard at the Behavioral Health Tech Conference
At BHT, everyone agreed that measurement matters. What was missing was the harder question: How do you ensure clinicians actually practice MBC? Clinician buy-in is one of the biggest hurdles — many were never taught MBC, worry it won’t capture the full story, or fear being judged by their scores. A single training can’t overcome those concerns.
This is where implementation science matters. You need a culture of psychological safety, real coaching, and a shared understanding of how measurement improves care. Without clinician engagement, clients won’t complete measures consistently, and the whole system collapses.
At Two Chairs, we use Dean Fixsen’s implementation science model, which identifies three core drivers of successful adoption:
- Competency: training, coaching, feedback
- Organization: infrastructure, policies, workflows, technology
- Leadership: culture, alignment, accountability
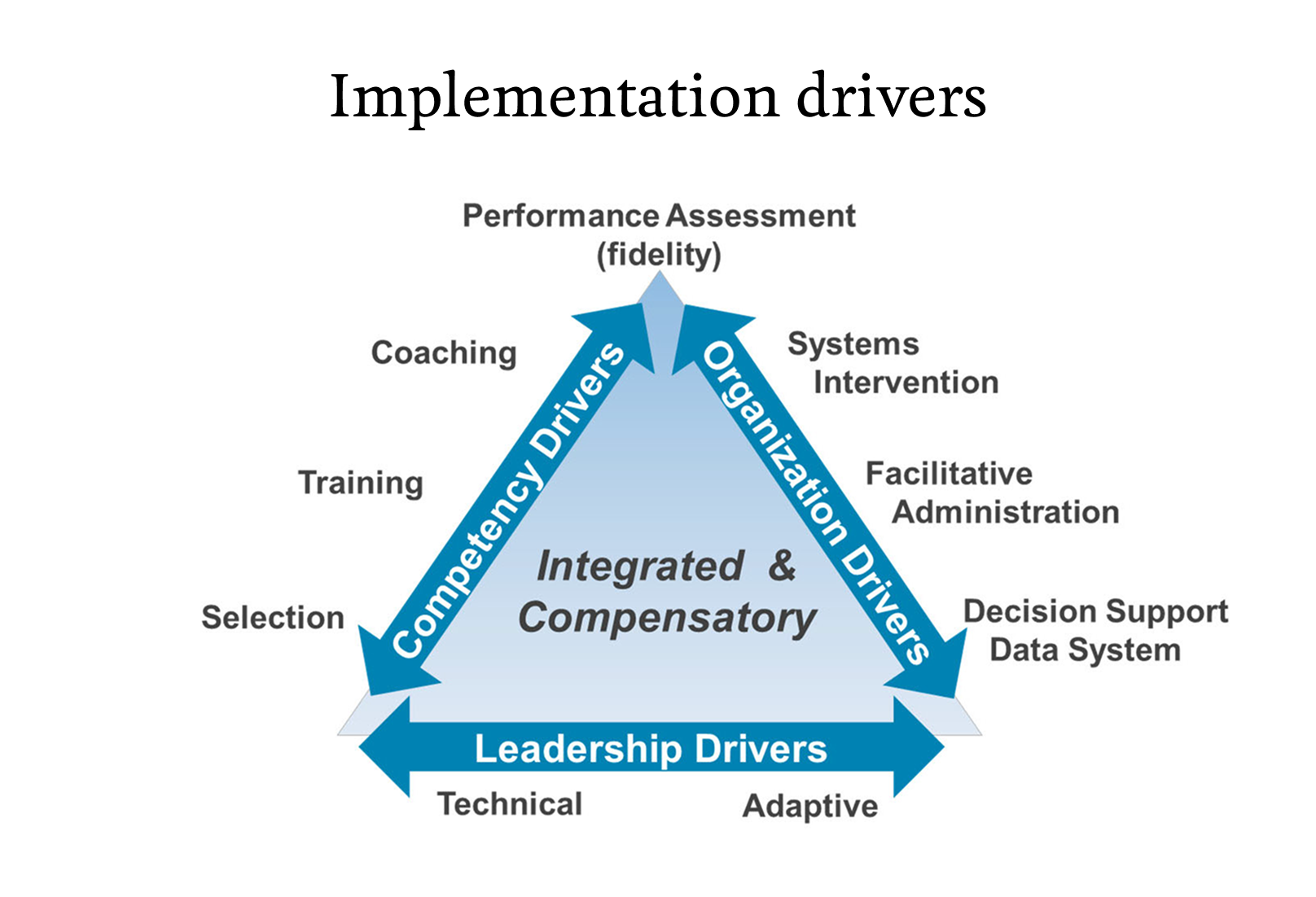
His framework makes one thing clear: implementation is the intervention. Collecting measures isn’t enough — you need infrastructure that reinforces the behaviors required for MBC to work. That part is almost entirely absent from today’s industry conversation, which is why so much MBC remains superficial.
Collecting Measures Is Not MBC
Many companies equate MBC with sending a PHQ-9 or GAD-7 survey and displaying the scores in a dashboard. That’s measurement — not measurement-based care.
MBC only exists when measures are reviewed collaboratively, used to guide treatment, and incorporated into clinical decision-making. That requires skill, and skill requires training, coaching, and deliberate practice.
Early in our own implementation, we saw the risks of getting it wrong. Some clinicians, anxious about alliance scores, encouraged clients to “give them a good rating.” That wasn’t a clinician problem — it was a systems problem. We removed alliance scores from performance metrics, rebuilt supervision, and doubled down on coaching the relational skills MBC requires. That’s what real implementation looks like.
Why 1099 Networks Cannot Deliver Real MBC
Many companies claiming to “deliver MBC at scale” rely on large 1099 contractor networks, but a 1099 model significantly limits the ability of an organization to:
- require training in a specific evidence-based practice, such as MBC.
- coach clinicians to skill acquisition.
- enforce workflows or documentation standards.
- align policies and procedures across hundreds or thousands of independent practitioners.
- build a feedback culture grounded in humility and growth when there is no shared leadership structure.
Even well-intentioned provider networks are structurally unable to implement true MBC. They can collect measures, but they are limited in their abilities to ensure they are used in care — nor can they produce consistent, population-level outcomes.
As I often tell payers: If you cannot enforce practice, you cannot promise outcomes.
What the New Two Chairs Study Shows
Our new study, “The Impact of Measurement Based Care at Scale,” evaluated our six-month MBC training and implementation program across 755 clinicians and 18,721 clients — one of the largest real-world MBC analyses to date.
Some of our key findings:
- Clinical outcomes improved by 24% after implementation
- 95% of clinicians who were present across the training period improved their patient outcomes
- MBC discussions in session increased from 79.8% to 96.2%
- Measures are collected in 95% of sessions, and 100% of clinicians use MBC
These results reflect behavioral change across an entire workforce — exactly what implementation science predicts when competency, organizational support, and leadership align.
Why Our Model Works
None of this is possible without a W-2 employment model. As employees, our clinicians can be selected, trained, coached, and supported within a consistent culture and infrastructure. This allows us to:
- Recruit clinicians who value measurement
- Train to skill, not just knowledge
- Align workflows and documentation
- Measure outcomes across the full population
- Invest long-term in research and quality
Most importantly, we can build a culture where MBC is embraced, not feared — a culture where feedback, transparency, and shared learning are the norm.
What This Means for the Future of Behavioral Health
Seeing this research published is deeply meaningful — not just for our clinical team, but for the broader field. It shows what MBC can achieve when it is implemented with rigor, fidelity, and respect for the science behind it.
The industry needs a more honest conversation about MBC. If we want to deliver mental health care that truly improves outcomes, strengthens the therapeutic relationship, and supports long-term healing, we must raise the bar.
We need implementation science.
We need training and accountability.
We need organizational structures that make quality possible.
And we need to stop pretending that collecting measures is the same as practicing measurement-based care.
This paper shows what’s possible when MBC is done right. My hope is that it pushes the field toward a higher standard — for payers, providers, and most importantly, for the people seeking care.





